Healthcare Then and Now: What We Can Learn From the Family Doctor of the Past
April 6th, 2021 | 5 min. read

Decades ago, healthcare looked vastly different than it does today. The family doctor knew and treated every member of the family, from birth to death. No matter the time of day, the doctor could be reached.
The amount of time spent with patients wasn’t measured. Excellent care and wellness were the primary objectives. Physicians sat down with patients, took the time to think through problems and used their breadth of knowledge to come up with a diagnosis. Back then, in addition to treating hypertension and diabetes, the doctor splinted sprained wrists, sutured lacerations and removed cysts – problems that would likely be referred out to urgent care centers or specialists today.
The doctor was free and independent and not employed by a health system or bogged down by overly burdensome regulations. Healthcare was between the doctor and recipients of care, and the doctor was truly an advocate for his or her patients.
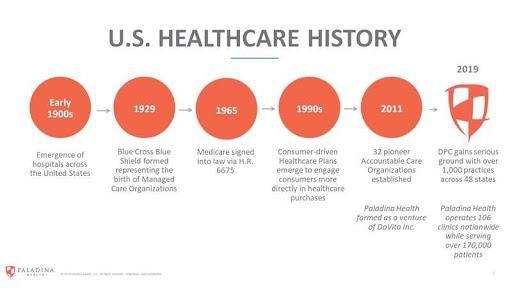
The early days of managed care
Several decades ago, the government began implementing interventions intended to address rising healthcare costs. One of the first was the introduction of the Health Maintenance Organization Act of 1973, which directly spurred the development of HMOs. The 1990s saw tremendous growth of private organizations and employer-sponsored HMOs, PPOs and physician hospital organizations (PHOs) in an effort to reduce costs by eliminating provider incentives for inappropriate care and excess use of services.
Many managed care organizations entered into capitated arrangements with contracted physicians during the 1990s. In these arrangements, providers would receive a fixed amount per member per month. Capitation was intended to emphasize primary care as central to improving healthcare and keeping hospital costs reigned in.
However, capitation created a perverse financial incentive to deny access to care and limit utilization, which was detrimental to patients. Because payment was not tied to outcomes, capitation arguably pressured providers to prioritize cutting spending over patient well-being. Eventually, benefit denials and disallowances of medically necessary services prompted a public outcry and the enactment of laws in many states establishing managed care standards.
By many accounts, managed care has contributed to a general deterioration of the relationship between doctor and patient, as well as decreased patient and physician satisfaction. Physicians complain of pressure to increase volume by restricting time spent with each patient. The vehicles of managed care dictate the limits of treatment with less regard for the judgement of the physician. This fee-for-service system, poorly constructed for the delivery of comprehensive primary care, incentivizes doctors to bill insurance based on every exam and procedure performed during a visit rather than to deliver holistic, high-value care.
Today: volume over value still prevails
Well into the 21st century, efforts to deliver better care at lower costs have largely failed. Healthcare costs still outpace general inflation. Despite reform initiatives aimed at shifting to value-based payment models, fee-for-service still dominates the U.S. healthcare industry. By and large, the system still rewards doing more (volume) rather than whatever would be the best, most appropriate course of care (value).
The demands on physician time continue to increase. On top of seeing more patients, computer work and administrative burdens have spiraled. The result is decreased face-to-face time with patients, leaving many primary care providers feeling like they are on an assembly line rather than engaged in a mission to heal the sick and prevent serious illness.
With the rise of consumerism in healthcare, patients are increasingly seeking a better and more convenient and individualized healthcare experience. Yet primary care remains difficult to access, with long wait times, short appointments, and limited alternative hours and appointment formats. These access challenges hamper the ability to establish close patient-provider relationships and achieve optimal health and wellness.
The stakes have never been higher to improve quality and outcomes and reduce costs. But can the healthcare of America’s future really become higher-performing, more patient-focused and less expensive?
Tomorrow: technology and a trip back in time
It’s no secret that our healthcare system has problems. For decades, Americans have been spending more on healthcare and getting less for their money. Despite devoting one-fifth of our economy to healthcare, Americans are not getting healthier. But a number of promising developments signal that change is on the horizon.
Care in the home
Technological advances are enabling more and more healthcare services to take place in the home. Remote monitoring tools can now monitor pulse, blood oxygenation levels, diet, glucose and blood pressure. Telehealth visits via video or phone connect doctors and patients to diagnose and treat health problems or help manage chronic conditions. Telemedicine is also solving access problems in rural areas, where a patient may have to drive hours to get to their doctor’s office.
Many of the challenges of aging in place, such as security, mobility and isolation, are being solved with technology as well. Telehealth, automated medication reminders and dispensers, and medical alert systems hold tremendous promise to help seniors remain independent and avoid or delay home health services or nursing facilities.
Value-based care
Today, value-based reimbursement is creating a paradigm shift in healthcare. The model is fundamentally transforming our century-old system for paying doctors for the care they provide. We’re moving from a healthcare system based on fee-for-service visits, tests and hospital admissions to one based on quality of care, health outcomes and patient satisfaction. Although the transition has been slower than expected, value-based care is showing promise when it comes to solving the cost and quality problems that have long-plagued the U.S. healthcare system.
Currently, hundreds of accountable care organizations that care for millions of patients are tying payments to quality of care, improved patient outcomes and better use of resources.
Direct Primary Care
Another force advancing the pursuit of higher quality care at lower costs is direct primary care (DPC). DPC bypasses health insurance, usually by charging a monthly membership fee rather than billing for each visit or procedure.
While individual patients can enter direct primary care arrangements and pay for them via monthly subscription, many DPC providers are funded by employers on a flat per-member-per-month basis. Employer-sponsored DPC is a powerful tool for managing healthcare costs and an attractive piece of an employee benefits package in a tight labor market.
Since direct primary care providers have smaller patient panels, the physician can spend more time on each visit, offer same-day appointments, and get to know patients well. The doctor no longer feels a need to run from room to room, seeing patients on a tight schedule, just to maintain stable revenues for the practice. The aim of direct primary care is long-term health and well-being, not simply the treatment of illness or injury. Where fee-for-service is reactive, DPC is proactive. Physicians can take a holistic approach to healthcare, addressing risk factors that lead to chronic conditions and caring for multiple issues in one visit.
Freed from insurance administrative burdens and rushing from one patient to another, doctors have the time and cognitive space to meet the vast majority of patients’ healthcare needs. If a referral to a specialist is needed, DPC physicians act as navigators and healthcare quarterbacks to identify the best providers based on quality and cost data.
Like the family doctor of yesterday, direct primary care providers do what is truly in the best interest of their patients. That means being available by phone at any time, which often eliminates the need for an urgent care or emergency room visit, or even the hassle of traveling for an in-person visit with their direct primary care provider. In a traditional practice, phone consultations typically aren’t available, largely because clinic visits are the only way a provider is reimbursed by insurance companies. Not tethered by these restrictions, DPC providers can be available by phone, video, or text at times convenient to the patient – whatever is needed to give them access to care when and where they need it.
Patients and doctors alike yearn for more convenient, direct and individualized care. Given the discontent with modern healthcare, promising new care models like direct primary care and healthcare delivered in the home are ideas whose time has come. The most viable emerging solutions are those that blend the best part of “old school” medicine with exciting advancements in technology, paving the way for unprecedented access and health outcomes. Interested in exploring how Everside’s direct primary care services might fit into your organization’s benefits offering?